Anatomy. Posterior malalignment of conal septum with muscular septum creates this constellation of anatomic findings (in some ways representing the posterior-deviated version of TOF). Conal septum crowds the LVOT, the AV is hypoplastic, and (presumably) diminished aortic flow in utero causes hypoplasia of the aortic arch. The aortic arch may exhibit coarctation at the isthmus (i.e. CoA/VSD) or may be nearly or completely interrupted. Anatomic subtypes describe the precise location of interruption. Aberrant subclavian ateries (from the DAo) may cause all measured BPs and SpO2s to be post-ductal.



Physiology. This circulation is PGE-dependent due to the interruption of the aorta. Impedance to flow into the aorta is significantly increased in this circulation, such that there is much more left to right ventricular shunting in this circulation than in the absence of aortic obstruction. This shunting of blood (LV to PA via the RVOT) significantly increases PA saturations and therefore post-ductal saturations (which can approach normal in settings of elevated Qp/Qs and/or low VO2). Post-ductal perfusion (exam, UOP, and if concerned creatinine, LFT) must be carefully monitored and a restrictive PDA ruled out.
Repair of VSD/IAA
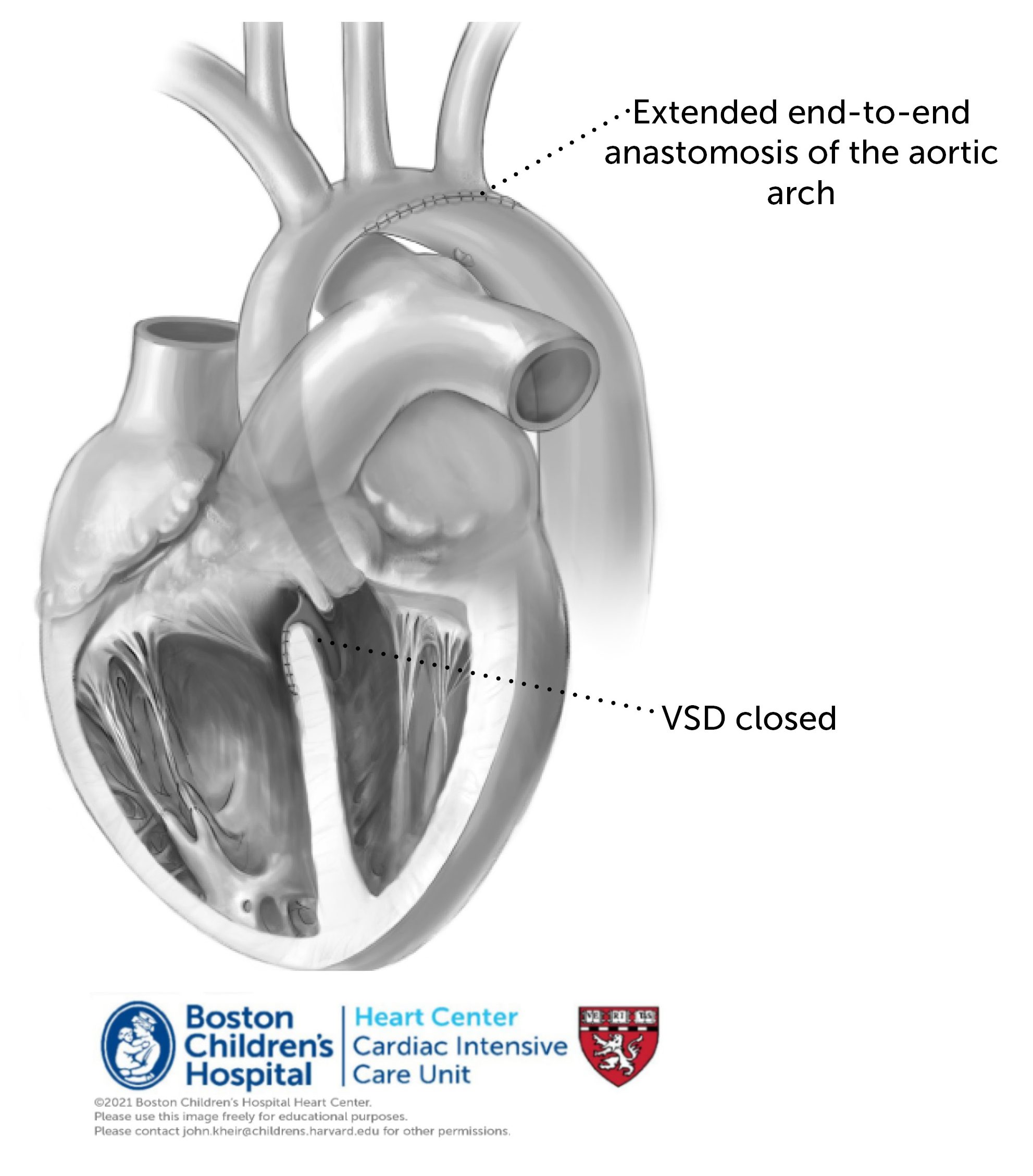
Repair. In most cases, corrective surgery is possible in the newborn period. This includes a reconstruction of the aortic arch (at times using homograft patch) as well as the closure of the VSD. In cases of prematurity or contraindication to neonatal surgery (e.g. cerebral hemorrhage, severe organ dysfunction), the circulation may be palliated using branch PA banding and maintaining ductal patency (PGE or ductal stenting). Postoperative considerations. In patients who are not intubated nor have organ dysfunction preoperatively, the postoperative course is generally smooth. The LV may exhibit restrictive physiology (e.g. elevated LA pressure with volume administration or valsalva). It is important to ensure sinus rhythm, monitor for junctional tachycardia, consider residual VSD (evaluate by echo or by RA-PA saturations in OR), which may be poorly tolerated in this circulation. Residual aortic arch obstruction is also rare but should be considered. Supportive care includes weaning from mechanical ventilation, inotropic support and diuresis. Patients who are more ill preoperatively may exhibit a prolonged postoperative course, particularly in the setting of renal or hepatic insufficiency.
References